Understanding Venous Stasis Causes: A Complete Guide to Vascular Health and Treatment

Vascular health plays a crucial role in maintaining overall well-being, ensuring that blood circulates efficiently throughout the body. Among the many vascular conditions, venous stasis is a common yet complex issue that results from various causes. Recognizing these causes is essential for early diagnosis, effective treatment, and preventing serious complications such as blood clots, ulcers, and chronic venous insufficiency.
What Is Venous Stasis?
Venous stasis refers to the impaired flow of blood through the veins, especially in the lower extremities. When blood stagnates or pools in the veins, it can lead to increased pressure, tissue damage, and a cascade of venous disorders. The condition is often associated with symptoms like swelling, skin discoloration, pain, and the formation of venous ulcers.
Why Are Understanding the Venous Stasis Causes So Important?
Identifying venous stasis causes is vital for clinicians to tailor appropriate treatment strategies. Understanding the underlying reasons enables targeted therapies that can restore proper blood flow, promote venous healing, and prevent recurrence. This knowledge also empowers patients to adopt lifestyle changes that mitigate risk factors associated with venous stasis.
Primary Causes of Venous Stasis
The causes of venous stasis are multifaceted, often involving a combination of anatomical, physiological, and lifestyle factors. The primary causes include:
- Chronic Venous Insufficiency (CVI): A condition where damaged venous valves fail to prevent backflow, leading to blood pooling.
- Venous Obstruction: Physical blockages such as deep vein thrombosis (DVT) impair blood flow, causing stasis.
- Valve Malfunction: Dysfunction or damage to venous valves, often due to inherited conditions or previous injuries.
- Venous Wall Abnormalities: Weak or damaged venous walls contribute to vein dilation and stasis.
- Prolonged Immobility: Extended periods of inactivity, such as bed rest or long flights, hinder muscle pump function that aids venous return.
- Obesity: Excess weight pressures the venous system, increasing stasis risk.
- Pregnancy: Hormonal changes and increased abdominal pressure promote venous pooling, especially in the lower limbs.
Secondary Causes of Venous Stasis
Aside from primary factors, secondary causes often compound the risk of venous stasis. These include:
- Certain Medications: Hormonal therapies and oral contraceptives can influence venous tone and flow.
- Trauma and Surgery: Injuries or surgical procedures in the lower extremities can damage venous structures, impairing blood flow.
- Lifestyle Factors: Sedentary habits, smoking, and poor diet negatively impact vascular health.
- Venous Malformations: Congenital abnormalities causing abnormal venous channels can predispose individuals to stasis.
Pathophysiology of Venous Stasis
The pathophysiological progression of venous stasis involves several interconnected mechanisms:
- Valve Dysfunction: Incompetent valves allow retrograde flow, leading to pooling of blood.
- Venous Dilation: Increased venous pressure causes veins to enlarge and become tortuous.
- Scarcity of Muscle Pumps: Reduced activity diminishes the calf muscle pump's effectiveness, impairing venous return.
- Capillary Leakage and Edema: Elevated venous pressure forces plasma out of capillaries, resulting in swelling and skin changes.
- Chronic Inflammation: Persistent venous hypertension stimulates inflammatory pathways, resulting in tissue damage and ulceration.
The Role of Medical Evaluation in Identifying venous stasis causes
A comprehensive medical assessment is essential for determining venous stasis causes. This involves:
- Detailed Patient History: Including symptoms, lifestyle habits, and family history.
- Physical Examination: Checking for edema, skin discoloration, varicose veins, and ulcers.
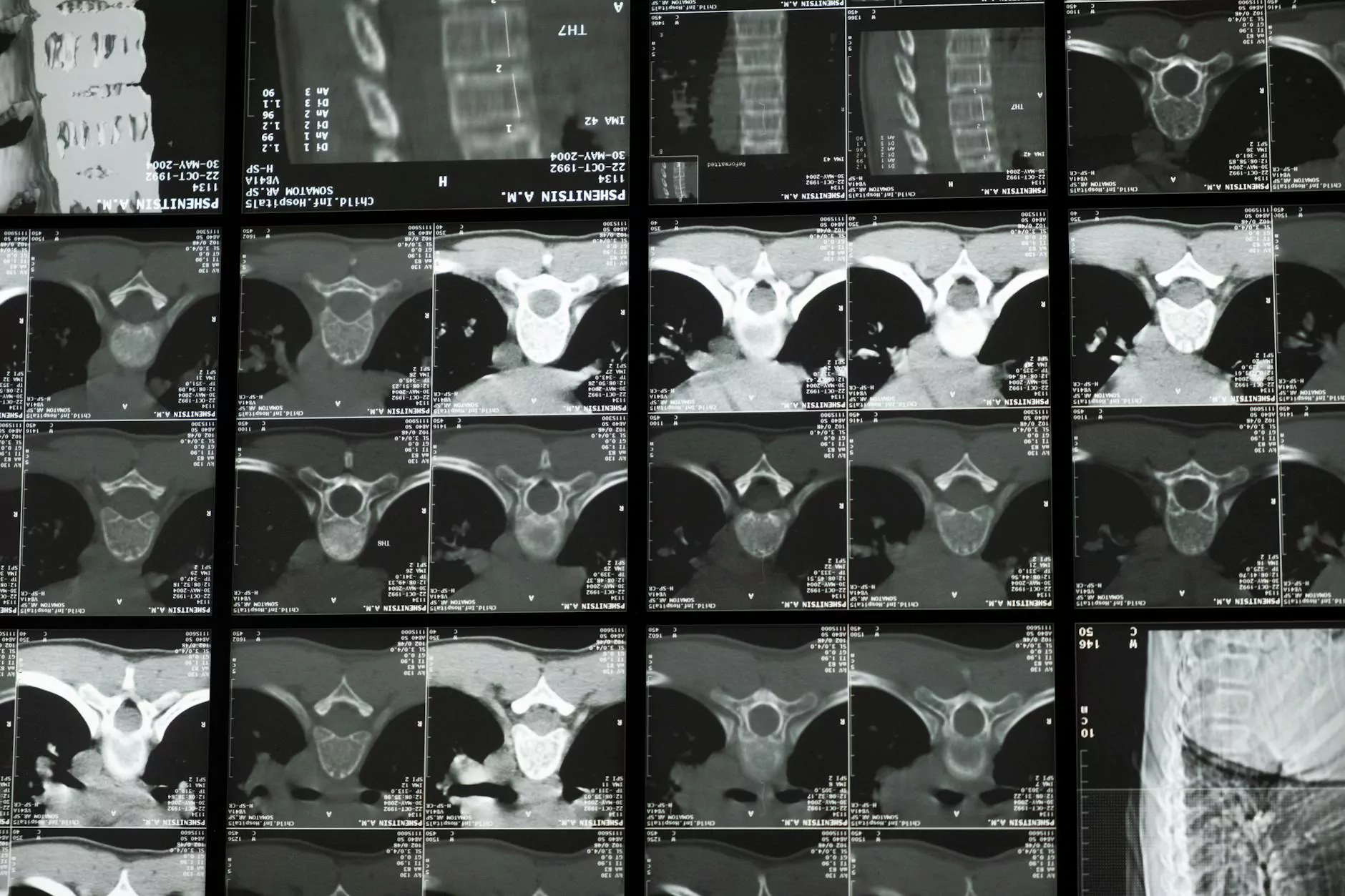
- Diagnostic Imaging: Venous Doppler ultrasound, venography, and other imaging techniques help visualize vein structure and flow dynamics.
- Laboratory Tests: To rule out clotting disorders or other systemic conditions.
Effective Treatment Strategies Addressing Venous Stasis Causes
Once the venous stasis causes are identified, tailored treatment plans can be implemented to improve vascular health. Treatment options include:
Conservative Management
- Compression Therapy: Compression stockings or wraps help reduce swelling and promote blood flow.
- Lifestyle Changes: Regular exercise, weight management, and avoiding prolonged immobility are crucial.
- Medication: Anti-inflammatory drugs, venotonic agents, and anticoagulants if thrombosis is present.
- Elevation: Elevating legs above heart level to facilitate venous drainage.
Interventional and Surgical Interventions
- Endovenous Laser Treatment (EVLT): Minimally invasive procedure to close incompetent veins.
- Sclerotherapy: Injecting sclerosant solution to obliterate abnormal veins.
- Veno-venous Bypass or Venous Stenting: Restoring flow in obstructed veins.
- Vein Valve Surgery: Repair or replacement of damaged valves in select cases.
Prevention and Long-Term Management of Venous Stasis
Prevention strategies focus on minimizing risk factors for venous stasis causes. These include:
- Maintaining a Healthy Weight: Reducing pressure on venous structures.
- Engaging in Regular Exercise: Activities like walking, swimming, and calf exercises strengthen the venous pump.
- Avoiding Prolonged Immobility: Taking breaks to move during long periods of sitting or standing.
- Using Compression Stockings: Especially for at-risk populations such as pregnant women or individuals with a history of venous disease.
- Monitoring and Managing Underlying Conditions: Diabetes, hypertension, and cardiovascular diseases should be well-controlled.
The Significance of Specialized Vascular Treatment
Addressing venous stasis causes requires expertise from highly trained vascular specialists. Clinics like Truffles Vein Specialists offer comprehensive diagnostics and personalized treatment plans. Their focus on Vascular Medicine ensures optimal outcomes for patients suffering from venous disorders.
Conclusion: Proactive Approach to Vascular Health
Understanding the causes of venous stasis is vital for effective prevention, diagnosis, and management. By actively addressing these causes through lifestyle modifications, medical interventions, and expert care, patients can significantly improve their quality of life and prevent serious complications associated with chronic venous disease.
At Truffles Vein Specialists, our dedicated team of Doctors and Vascular Medicine professionals are committed to providing world-class care tailored to your unique needs. Early detection and targeted treatment of venous stasis causes pave the way for healthier veins and a more vibrant life.